Endometriosis And PCOS
Share
Endometriosis and Polycystic Ovary Syndrome (PCOS) are two common conditions that affect many women of reproductive age. Both can cause a range of symptoms and complications, including infertility. Understanding these conditions, their differences, and how they can coexist is crucial for effective management and treatment.
Key Takeaways
- Endometriosis involves the growth of tissue similar to the lining of the uterus in other parts of the body, causing pain and potential infertility.
- PCOS is a hormonal disorder characterized by high levels of androgens, irregular menstrual cycles, and cysts in the ovaries.
- Both conditions can coexist, with women having an increased risk of endometriosis if they have PCOS.
- Diagnosing endometriosis often requires more complex procedures compared to PCOS, which can usually be diagnosed through a combination of physical exams, ultrasounds, and blood tests.
- Treatment for both conditions may include medication, lifestyle changes, and in some cases, surgery to manage symptoms and improve quality of life.
Understanding Endometriosis and PCOS
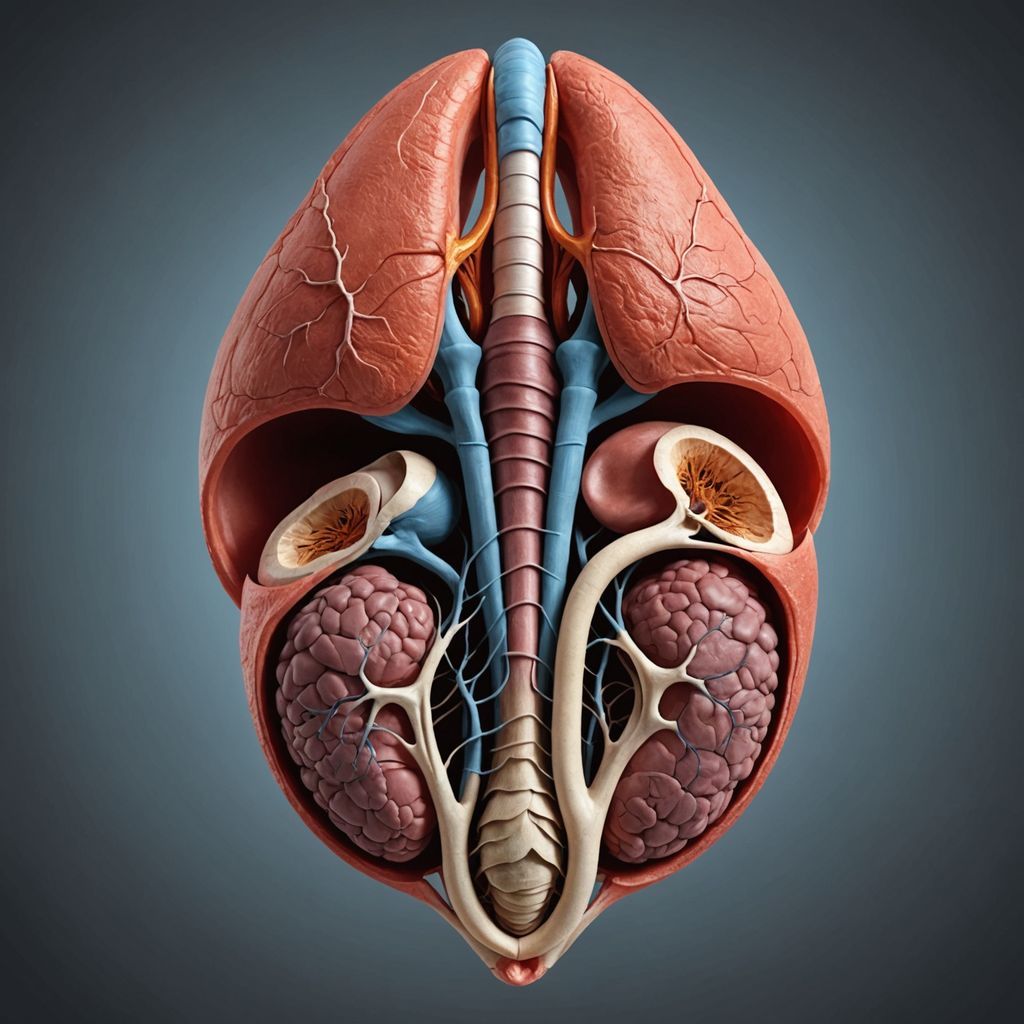
Definition of Endometriosis
Endometriosis is a condition where tissue similar to the lining inside the uterus, known as the endometrium, starts to grow outside the uterus. This tissue can be found on the ovaries, fallopian tubes, and other areas within the pelvic cavity. This abnormal growth can cause pain, inflammation, and infertility. The exact cause of endometriosis is not well understood, but factors like genetics and immune system issues may play a role.
Definition of PCOS
Polycystic Ovary Syndrome (PCOS) is a hormonal disorder common among women of reproductive age. It is characterized by the ovaries producing an excess amount of androgens, which are male hormones present in small amounts in women. This hormonal imbalance can lead to irregular menstrual cycles, infertility, and the development of cysts in the ovaries. The exact cause of PCOS is also not fully understood, but it is believed to involve a combination of genetic and environmental factors.
Prevalence and Demographics
Endometriosis affects approximately 10 to 15 percent of women of reproductive age. It is a significant cause of chronic pelvic pain and can severely impact quality of life. On the other hand, PCOS affects about 5 to 20 percent of women of childbearing age. It is one of the most common causes of infertility due to hormonal changes. Both conditions can coexist, and studies have shown that women with PCOS may also have unrecognized endometriosis. Managing these conditions often involves lifestyle changes and medical treatments to alleviate symptoms.
Symptoms and Clinical Manifestations

Common Symptoms of Endometriosis
Endometriosis is primarily marked by chronic pelvic pain and painful, heavy periods. Other symptoms include:
- Abdominal pain
- Painful bowel movements
- Painful urination
- Painful sex
- Infertility
- Heavy periods
- Frequent urination
- Constipation
- Rectal bleeding
- Urinary urgency
Common Symptoms of PCOS
PCOS symptoms are more systemic and include:
- Irregular or infrequent periods
- Excess body and facial hair
- Scalp hair loss
- Discolored skin patches in the armpits or under the breasts (acanthosis nigricans)
- Oily skin that is susceptible to acne
- Fluid-filled sacs in the ovaries
- Obesity
- Diabetes and insulin resistance
- Infertility
Differential Symptoms
While both conditions can result in painful cramps and cause infertility, there are other symptoms to keep in mind. Severe pain during periods, or dysmenorrhea, is a common sign of endometriosis. Those with PCOS may miss their period due to an inability to create enough hormones to ovulate. Having increased amounts of androgen could lead to other health problems such as type 2 diabetes, high blood pressure, or uterine cancer.
Causes and Risk Factors
Etiology of Endometriosis
The exact cause of endometriosis remains uncertain. However, several theories have been proposed:
- Retrograde menstruation: Menstrual blood flows backward through the fallopian tubes into the pelvic cavity.
- Genetic factors: A family history of endometriosis increases the risk.
- Immune system issues: An impaired immune system may fail to eliminate endometrial cells outside the uterus.
- High estrogen levels: Elevated estrogen can stimulate the growth of endometrial tissue.
- Surgical transfer: Endometrial cells may be transferred to other organs during abdominal surgeries.
Risk factors for endometriosis include:
- Early onset of menstruation (before age 11)
- Family history of endometriosis
- Short menstrual cycles (27 days or less)
- Heavy menstrual bleeding
- Infertility
- High estrogen levels
- Alcohol consumption
Etiology of PCOS
Polycystic Ovary Syndrome (PCOS) is a complex endocrine disorder with multiple contributing factors:
- Hormonal imbalance: High levels of androgens disrupt normal ovarian function.
- Insulin resistance: Inefficient use of insulin can lead to elevated insulin levels, which in turn increase androgen production.
- Inflammation: Chronic inflammation is linked to higher androgen levels.
- Genetic predisposition: A family history of PCOS can increase the likelihood of developing the condition.
Risk factors for PCOS include:
- Obesity
- Diabetes
- Epilepsy
- Hyperandrogenism
- Family history of PCOS
- Early onset of puberty (before age 8 or 9)
Shared and Unique Risk Factors
While endometriosis and PCOS have distinct causes, they share some common risk factors, such as hormonal imbalances and family history. However, each condition also has unique risk factors:
- Endometriosis: Early menarche, short menstrual cycles, and heavy bleeding.
- PCOS: Obesity, insulin resistance, and early puberty.
Understanding these causes and risk factors is crucial for early diagnosis and effective management of both conditions.
Diagnosis and Diagnostic Challenges
Diagnostic Methods for Endometriosis
Diagnosing endometriosis can be complex and often requires multiple steps. Initially, a healthcare provider will review the patient's medical history and conduct a physical exam to feel for cysts or scars behind the uterus. Imaging tests, such as ultrasounds or MRI scans, are used to identify larger areas of endometriosis, like cysts or nodules. Definitive diagnosis is only possible through laparoscopy, a surgical procedure where a small viewing instrument is inserted into the abdomen to check for endometrial tissue. A biopsy may be required to confirm the diagnosis.
Diagnostic Methods for PCOS
PCOS diagnosis typically involves ruling out other conditions and identifying specific symptoms. A healthcare provider will look for irregular or infrequent periods, high levels of androgens, and multiple cysts on the ovaries. Blood tests are used to confirm elevated androgen levels, while a pelvic ultrasound can help find ovarian cysts. Meeting two out of three of the Rotterdam Criteria—irregular menstrual periods, high testosterone levels, or polycystic ovaries on ultrasound—can confirm a PCOS diagnosis.
Challenges in Differential Diagnosis
Differentiating between endometriosis and PCOS can be challenging due to overlapping symptoms. Both conditions can cause pelvic pain and irregular menstrual cycles. However, endometriosis often involves physical distortions of the reproductive tract, while PCOS is primarily related to hormonal imbalances. The complexity of diagnosing endometriosis, which often requires surgical intervention, contrasts with the relatively straightforward process for diagnosing PCOS. The NIH has launched a new federal challenge to seek innovations in the diagnosis of endometriosis to broaden accessibility and improve women's health.
Treatment Approaches

Medical Treatments for Endometriosis
Treatment for endometriosis often focuses on managing pain and considering the individual's desire for pregnancy. Medications are commonly used, including nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce inflammation and pain. Hormonal treatments, such as Myfembree and Orilissa, and non-hormonal options like aromatase inhibitors, can also help alleviate symptoms. In some cases, surgery may be necessary to remove endometrial tissue or, in severe cases, the uterus, fallopian tubes, and ovaries. Lifestyle changes, such as eating more fresh fruits and vegetables and reducing gluten and dairy, have been shown to improve symptoms.
Medical Treatments for PCOS
PCOS treatment aims to manage symptoms and reduce long-term health risks like diabetes and heart disease. Medications such as oral contraceptives and antiandrogens help lower androgen levels and alleviate symptoms. Lifestyle changes, including weight loss and regular exercise, are often the first line of treatment. Losing 5% to 7% of body weight can help regulate menstrual cycles and improve fertility. Other treatments may include insulin-sensitizing agents like metformin and medications for specific symptoms such as acne or hair loss.
Surgical and Lifestyle Interventions
For endometriosis, surgery may involve removing endometrial tissue from various organs or, in severe cases, performing a hysterectomy. However, endometriosis can recur after surgery. Lifestyle changes, such as a healthy diet and regular exercise, can also help manage symptoms. For PCOS, lifestyle interventions are crucial. Weight loss and exercise can improve insulin sensitivity and hormone balance, helping to regulate menstrual cycles and improve overall well-being. In some cases, medications to induce ovulation may be recommended, though they come with risks like pelvic pain and bloating.
Impact on Fertility

Endometriosis and Infertility
Endometriosis is a condition where tissue similar to the lining inside the uterus grows outside of it. This can lead to inflammation, scarring, and adhesions, which can affect fertility. Approximately 30% to 50% of individuals with endometriosis experience infertility. The severity of endometriosis often correlates with the degree of infertility, making early diagnosis and treatment crucial.
PCOS and Infertility
Polycystic Ovary Syndrome (PCOS) is a hormonal disorder that affects ovulation. The primary cause of infertility in individuals with PCOS is the absence of ovulation. Around 70% to 80% of people with PCOS face infertility issues. Lifestyle changes, such as weight loss and exercise, can help regulate menstrual cycles and improve fertility. Medications like letrozole, clomiphene, and metformin are often prescribed to stimulate ovulation.
Managing Fertility Issues
Managing fertility issues in individuals with endometriosis or PCOS often requires a multifaceted approach. For endometriosis, surgical intervention by an experienced gynecologic surgeon can remove endometrial tissue and improve fertility outcomes. In cases where surgery is not sufficient, assisted reproductive technologies like in vitro fertilization (IVF) may be recommended.
For PCOS, lifestyle modifications are the first line of treatment. Weight loss and regular exercise can significantly improve ovulation and fertility. If lifestyle changes are not effective, medications to induce ovulation are considered. In some cases, IVF may also be an option.
Both conditions require ongoing management and consultation with healthcare professionals to optimize fertility outcomes. Early diagnosis and tailored treatment plans are essential for improving the chances of conception.
Coexistence of Endometriosis and PCOS
Prevalence of Coexistence
Although it is uncommon, it is possible for individuals to have both endometriosis and PCOS simultaneously. Research indicates that a notable number of women with PCOS may also have undiagnosed endometriosis. Studies have shown that increased inflammation, high androgen levels, and insulin resistance in PCOS can elevate the risk of developing endometriosis. For instance, a 2014 study found that many women with PCOS also had stage I or stage II endometriosis lesions.
Clinical Implications
The coexistence of endometriosis and PCOS can complicate the clinical picture, making diagnosis and treatment more challenging. Women with both conditions may experience a combination of symptoms from each disorder, such as irregular menstrual cycles, pelvic pain, and infertility. The overlapping symptoms can sometimes lead to misdiagnosis or delayed diagnosis, affecting the overall management and quality of life for these patients.
Management Strategies
Managing both endometriosis and PCOS requires a comprehensive approach that addresses the symptoms and underlying causes of both conditions. Treatment plans may include:
- Medical Treatments: Hormonal therapies to regulate menstrual cycles and reduce pain and inflammation.
- Surgical Interventions: Procedures like laparoscopy to remove endometrial lesions.
- Lifestyle Modifications: Diet and exercise to manage weight and improve insulin sensitivity.
A multidisciplinary team, including gynecologists, endocrinologists, and nutritionists, can provide a more effective treatment plan tailored to the individual's needs.
Conclusion
Endometriosis and PCOS are two distinct yet sometimes overlapping conditions that significantly impact women's reproductive health. Both can lead to infertility, though through different mechanisms—hormonal imbalances in PCOS and physical distortions in endometriosis. While each condition has its own set of symptoms and diagnostic criteria, they can coexist, complicating diagnosis and treatment. Early detection and specialized care are crucial for managing symptoms and improving quality of life. Regular gynecological checkups and consultations with specialists are essential for those experiencing symptoms or having difficulty conceiving. Understanding these conditions better can lead to more effective treatments and improved outcomes for affected individuals.
Frequently Asked Questions
What is endometriosis?
Endometriosis is a condition where tissue similar to the lining inside the uterus starts to grow outside the uterus. This can cause pain, especially during periods, and may lead to infertility.
What is PCOS?
PCOS, or Polycystic Ovary Syndrome, is a hormonal disorder causing enlarged ovaries with small cysts on the outer edges. It can lead to irregular menstrual cycles, excess hair growth, acne, and obesity.
Can endometriosis and PCOS affect fertility?
Yes, both conditions can impact fertility. PCOS can cause hormonal imbalances that interfere with ovulation, while endometriosis can cause physical changes in the reproductive tract that make it harder to conceive.
Can you have both endometriosis and PCOS at the same time?
Yes, it is possible to have both conditions simultaneously. Some studies suggest that women with PCOS may have a higher risk of also having endometriosis.
How are endometriosis and PCOS diagnosed?
PCOS is usually diagnosed through a pelvic exam, ultrasound, and blood tests to check hormone levels. Endometriosis is more complex to diagnose and often requires imaging tests and sometimes a laparoscopy to confirm.
Are the treatments for endometriosis and PCOS different?
Yes, treatments differ. Endometriosis treatment often focuses on pain relief and reducing estrogen levels, while PCOS treatment may include lifestyle changes, medications to regulate menstrual cycles, and treatments for insulin resistance.
