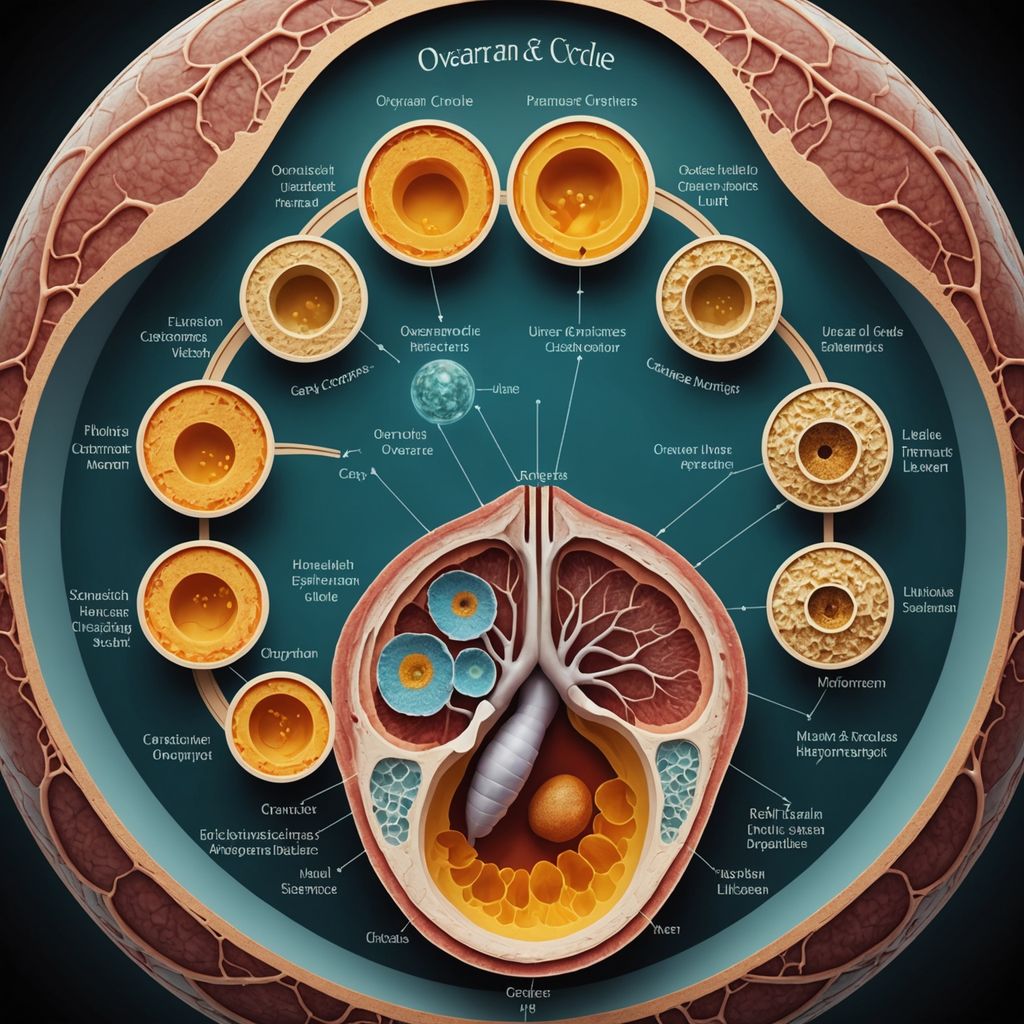
Ovarian cycle
Share
The ovarian cycle is a series of events that occur in the female reproductive system to prepare for the possibility of pregnancy. This cycle involves the development and release of an egg from the ovaries and the preparation of the uterine lining for potential implantation. The ovarian cycle is crucial for reproduction and is regulated by various hormones.
Key Takeaways
- The ovarian cycle consists of three main phases: the follicular phase, ovulation, and the luteal phase.
- Hormones like GnRH, FSH, and LH play essential roles in regulating the ovarian cycle.
- Ovarian follicles develop through stages, including primordial, primary, secondary, and antral follicles.
- The ovarian and menstrual cycles are synchronized and influence each other.
- Clinical aspects of the ovarian cycle, such as anovulatory cycles and short luteal phases, can impact fertility.
Phases of the Ovarian Cycle

The ovarian cycle is a recurring process that prepares the female body for potential pregnancy. It typically spans 28 days and is divided into three distinct phases: the follicular phase, ovulation, and the luteal phase. Each phase plays a crucial role in the maturation and release of an oocyte, as well as the preparation of the uterus for possible implantation.
Follicular Phase
The follicular phase marks the beginning of the ovarian cycle. It starts on the first day of menstruation and lasts until ovulation, averaging about 14 days. During this phase, ovarian follicles mature under the influence of follicle-stimulating hormone (FSH). The dominant follicle eventually emerges, preparing to release an oocyte. Estrogen levels rise, leading to the thickening of the uterine lining.
Ovulation
Ovulation occurs around the midpoint of the cycle, typically on the 14th day. Triggered by a surge in luteinizing hormone (LH), the dominant follicle releases a mature oocyte into the fallopian tube. This is the period when a woman is most fertile. The oocyte remains viable for about 24 hours, awaiting fertilization.
Luteal Phase
Following ovulation, the luteal phase begins and lasts until the start of the next menstrual period, approximately 14 days. The ruptured follicle transforms into the corpus luteum, which secretes progesterone. Progesterone prepares the uterine lining for potential implantation of an embryo. If fertilization does not occur, the corpus luteum degenerates, leading to a drop in hormone levels and the onset of menstruation. This phase is critical for maintaining the menstrual cycle's regularity and is often monitored in fertility treatments, including the use of period underwear for women.
Hormonal Regulation of the Ovarian Cycle

Role of Gonadotropin-Releasing Hormone (GnRH)
Gonadotropin-Releasing Hormone (GnRH) is secreted by the hypothalamus. This hormone plays a crucial role in the ovarian cycle by stimulating the pituitary gland to release two other important hormones: Follicle-Stimulating Hormone (FSH) and Luteinizing Hormone (LH). The release of GnRH is regulated by a feedback mechanism involving estrogen and progesterone levels in the blood. GnRH is essential for the proper functioning of the ovarian cycle.
Function of Follicle-Stimulating Hormone (FSH)
Follicle-Stimulating Hormone (FSH) is released by the pituitary gland in response to GnRH. FSH is responsible for the growth and maturation of ovarian follicles. As the follicles develop, they begin to secrete estrogen, which further regulates the release of FSH through a feedback loop. The role of FSH is vital in preparing the follicles for ovulation.
Impact of Luteinizing Hormone (LH)
Luteinizing Hormone (LH) is also released by the pituitary gland and works closely with FSH. The surge in LH levels triggers ovulation, the release of a mature egg from the dominant follicle. After ovulation, LH supports the formation of the corpus luteum, which secretes progesterone to maintain the uterine lining for potential pregnancy. The impact of LH is significant in both ovulation and the luteal phase of the ovarian cycle.
Ovarian Follicle Development
Primordial Follicles
Primordial follicles are the initial stage of ovarian follicle development. These follicles consist of an immature ovum surrounded by a single layer of granulosa cells. At this stage, the oocytes are in a dormant state, awaiting signals to begin maturation. The majority of these follicles will not progress beyond this stage and will undergo atresia, a process of programmed cell death.
Primary and Secondary Follicles
When stimulated by follicle-stimulating hormone (FSH), some primordial follicles develop into primary follicles. These primary follicles have a larger oocyte and multiple layers of granulosa cells. As they continue to grow, they become secondary follicles, characterized by the formation of a fluid-filled cavity called the antrum. The secondary follicles also develop a thecal cell layer, which plays a crucial role in hormone production.
Antral Follicles
Antral follicles, also known as tertiary follicles, are the next stage in follicle development. These follicles have a well-defined antrum and a highly differentiated wall consisting of theca externa, theca interna, and granulosa cells. Under the influence of luteinizing hormone (LH) and FSH, antral follicles produce and secrete estrogens. Typically, only one antral follicle will reach full maturity and be selected for ovulation, while the others undergo atresia.
Interplay Between Ovarian and Menstrual Cycles
Synchronization of Cycles
The ovarian and menstrual cycles are closely linked, occurring simultaneously over a typical 28-day period. The ovarian cycle prepares the ovaries to release an egg, while the menstrual cycle readies the uterine lining for potential pregnancy. Both cycles are synchronized to ensure optimal conditions for fertilization and implantation. If fertilization does not occur, the cycles reset, starting anew.
Hormonal Interactions
Hormones play a crucial role in coordinating the ovarian and menstrual cycles. The hypothalamus releases gonadotropin-releasing hormone (GnRH), which prompts the pituitary gland to secrete follicle-stimulating hormone (FSH) and luteinizing hormone (LH). These hormones regulate the growth of ovarian follicles and the release of an egg. Estrogen and progesterone, produced by the ovaries, further influence the thickening and shedding of the uterine lining.
Impact on Uterine Lining
The uterine lining, or endometrium, undergoes significant changes throughout the menstrual cycle. During the follicular phase, rising estrogen levels cause the endometrium to thicken, preparing for a potential pregnancy. After ovulation, progesterone maintains the endometrium. If pregnancy does not occur, hormone levels drop, leading to the shedding of the uterine lining during menstruation. This cyclical process is essential for reproductive health and is supported by products like period underwear for women, which offer comfort and protection during menstruation.
Clinical Aspects of the Ovarian Cycle
Anovulatory Cycles
Anovulatory cycles are menstrual cycles where ovulation does not occur. This condition is common in young girls who have just started menstruating and in women approaching menopause. Approximately one-third of menstrual cycles are anovulatory. Factors such as stress, anxiety, and eating disorders can disrupt the hormonal balance, leading to anovulation. Chronic anovulation affects 6-15% of women during their reproductive years and can be a sign of underlying conditions like polycystic ovary syndrome (PCOS). Despite being a common occurrence, anovulatory cycles can impact fertility and overall menstrual health.
Short Luteal Phases
A short luteal phase is characterized by a luteal phase lasting less than ten days. This phase is crucial for progesterone production, which supports the uterine lining for potential pregnancy. When the luteal phase is too short, progesterone levels are insufficient, affecting normal physiology and fertility. Short luteal phases can occur due to hormonal imbalances, stress, or intense physical activity. These changes are often reversible once the underlying stressors are managed or the body adapts to new physical demands.
Implications for Fertility
Both anovulatory cycles and short luteal phases have significant implications for fertility. Without ovulation, there is no egg available for fertilization, making conception impossible. Similarly, a short luteal phase can prevent the uterine lining from being adequately prepared for implantation, reducing the chances of a successful pregnancy. Women experiencing these issues may benefit from medical evaluation and treatment to address hormonal imbalances and improve their reproductive health. For those seeking non-invasive options, the New York Times's Top pick Period underwear for women can offer comfort and support during irregular cycles.
Ovarian Cycle Across the Lifespan

Cycle Changes at Puberty
The onset of puberty marks the beginning of the ovarian cycle. During this time, a child's body matures into an adult body capable of reproduction. The first menstrual period, known as menarche, typically occurs around the age of 12. Initially, the cycles may be irregular as the body adjusts to the new hormonal changes. Gradually, the cycles become more regular as the hormonal interplay stabilizes.
Cycle Variations During Reproductive Years
Throughout the reproductive years, the ovarian cycle follows a more predictable pattern. The cycle, which averages 28 days, consists of the follicular phase, ovulation, and the luteal phase. However, factors such as stress, diet, and overall health can cause variations. Anovulatory cycles, where ovulation does not occur, are not uncommon and can be influenced by external factors. The regularity of the cycle is a key indicator of reproductive health.
Cycle Cessation at Menopause
Menopause signifies the end of the ovarian cycle and typically occurs between the ages of 45 and 55. This phase is characterized by the cessation of menstrual periods and a significant decline in hormone levels. The transition to menopause, known as perimenopause, can last several years and is marked by irregular cycles and symptoms such as hot flashes and mood swings. The relationship between ovarian aging and senescent cell accumulation is a topic of ongoing research, with studies exploring the potential of senolytics to improve reproductive health.
Conclusion
The ovarian cycle is a fundamental aspect of female reproductive health, involving a series of well-coordinated phases that prepare the body for potential pregnancy. Understanding these phases—the follicular phase, ovulation, and the luteal phase—provides insight into how the body regulates fertility and menstrual health. Each phase is driven by hormonal changes that ensure the maturation and release of an egg, as well as the preparation of the uterine lining for possible implantation. This cyclical process not only highlights the complexity of the female reproductive system but also underscores the importance of hormonal balance in maintaining reproductive health. By studying the ovarian cycle, we gain a deeper appreciation for the intricate biological processes that support human life.
Frequently Asked Questions
What is the ovarian cycle?
The ovarian cycle is a series of events in the ovaries that prepare an egg for release and possible fertilization. It includes three main phases: the follicular phase, ovulation, and the luteal phase.
What happens during the follicular phase?
During the follicular phase, which starts on the first day of menstruation, follicles in the ovary grow and mature. This phase lasts about 14 days and ends with ovulation.
What is ovulation?
Ovulation is the release of a mature egg from the ovary. It usually happens around the middle of the cycle, about day 14 in a 28-day cycle.
What occurs in the luteal phase?
In the luteal phase, the empty follicle transforms into the corpus luteum, which produces hormones like progesterone to prepare the uterus for a possible pregnancy. If pregnancy doesn't occur, this phase ends with menstruation.
How is the ovarian cycle regulated by hormones?
The ovarian cycle is controlled by hormones such as GnRH, FSH, and LH. These hormones help in the growth of follicles, the release of the egg, and the preparation of the uterus for pregnancy.
How does the ovarian cycle change with age?
The ovarian cycle changes throughout a woman's life. It starts at puberty, becomes regular during the reproductive years, and eventually stops at menopause.
