Ovarian Cycle: Understanding The Monthly Changes
Share
The ovarian cycle is a key part of the female reproductive system, occurring every month. It involves several phases that prepare the body for potential pregnancy. Understanding this cycle helps us grasp how hormones and physical changes work together to support reproduction. In this article, we will explore the various phases of the ovarian cycle, how hormones regulate these changes, and their implications for health and fertility.
Key Takeaways
- The ovarian cycle lasts about 28 days and has three main phases: follicular, ovulation, and luteal.
- Hormones like FSH and LH play crucial roles in developing eggs and regulating the cycle.
- The follicular phase is when eggs mature, while ovulation is when an egg is released.
- The luteal phase prepares the uterus for a possible pregnancy with hormone production.
- Understanding the ovarian cycle is important for recognizing reproductive health issues and fertility treatments.
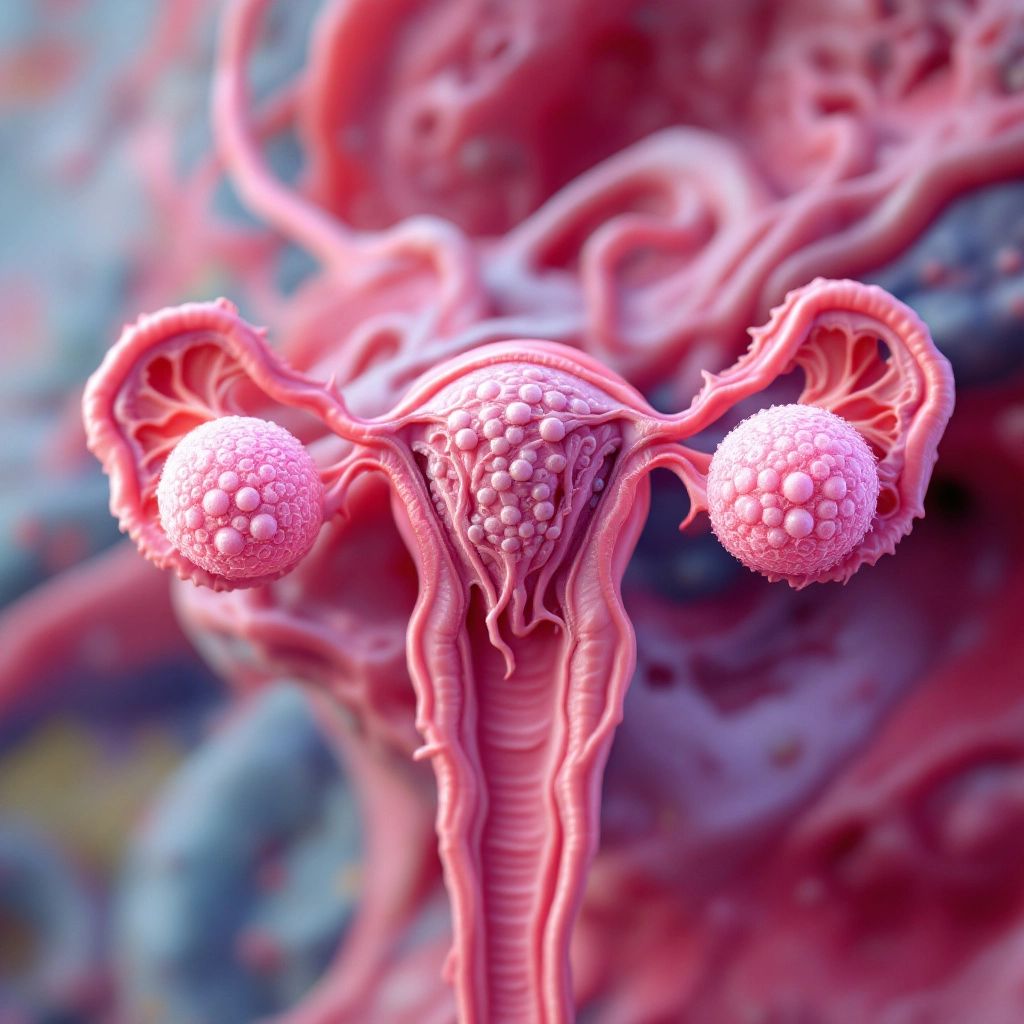
Phases of the Ovarian Cycle

The ovarian cycle is a crucial part of female reproductive health, typically lasting about 28 days. It consists of three main phases: the follicular phase, ovulation, and the luteal phase.
Follicular Phase
This phase marks the beginning of the ovarian cycle. It starts on the first day of menstruation and lasts until ovulation, usually around 14 days. During this time, several ovarian follicles begin to mature. The key events include:
- Development of multiple follicles: Several follicles grow, but usually only one becomes dominant.
- Hormonal changes: Follicle-stimulating hormone (FSH) levels rise, promoting follicle growth.
- Estrogen production: As follicles mature, they secrete estrogen, which helps prepare the body for ovulation.
Ovulation
Ovulation occurs approximately on the 14th day of the cycle. This is when the dominant follicle releases an egg. Key points include:
- LH Surge: A sudden increase in luteinizing hormone (LH) triggers the release of the egg.
- Egg Release: The egg is expelled from the ovary and enters the fallopian tube, where it may be fertilized.
- Follicle Transformation: The remaining follicle transforms into the corpus luteum after releasing the egg.
Luteal Phase
Following ovulation, the luteal phase lasts about 14 days. This phase is characterized by:
- Corpus Luteum Formation: The ruptured follicle becomes the corpus luteum, which produces progesterone.
- Hormonal Regulation: Progesterone prepares the uterine lining for a potential pregnancy.
- Cycle Reset: If fertilization does not occur, the corpus luteum degenerates, leading to a drop in hormone levels and the start of a new menstrual cycle.
In summary, the ovarian cycle is a complex interplay of hormonal changes and physiological events that prepare the female body for potential reproduction.
Hormonal Regulation of the Ovarian Cycle
The ovarian cycle is intricately controlled by hormones that ensure the proper functioning of the reproductive system. These hormones are essential for regulating the menstrual cycle and include key players such as FSH, LH, estrogen, and progesterone.
Role of FSH and LH
Follicle Stimulating Hormone (FSH) and Luteinizing Hormone (LH) are produced by the pituitary gland. Their roles include:
- FSH stimulates the growth of ovarian follicles.
- LH triggers ovulation and the formation of the corpus luteum.
- Both hormones work together to regulate the menstrual cycle.
Estrogen and Progesterone Dynamics
Estrogen and progesterone are produced by the ovaries and play crucial roles in the ovarian cycle:
- Estrogen promotes the growth of the uterine lining.
- Progesterone prepares the endometrium for potential implantation of a fertilized egg.
- The balance between these hormones is vital for maintaining reproductive health.
Feedback Mechanisms
The hormonal regulation of the ovarian cycle involves feedback mechanisms:
- Negative feedback: High levels of estrogen and progesterone inhibit the release of GnRH, FSH, and LH.
- Positive feedback: A surge in estrogen levels leads to a spike in LH, resulting in ovulation.
- This interplay ensures that the cycle progresses smoothly, allowing for the possibility of pregnancy.
In summary, the ovarian cycle is a complex interplay of hormones that regulate the menstrual cycle, ensuring the female body is prepared for potential pregnancy. Understanding these hormonal changes is crucial for recognizing menstrual cycle variations and their implications for reproductive health.
Follicular Development and Selection

Stages of Follicular Growth
The ovarian cycle begins with the growth of follicles, which are fluid-filled sacs that contain immature eggs. The process can be broken down into several key stages:
- Primordial Follicle Stage: This is the initial stage where immature eggs are surrounded by a layer of flat cells.
- Primary Follicle Stage: The flat cells become cuboidal, and the follicle begins to grow.
- Secondary Follicle Stage: The follicle continues to grow, and fluid-filled spaces start to form.
- Tertiary Follicle Stage: This is the final stage before ovulation, where the follicle is fully developed and ready to release an egg.
Dominant Follicle Selection
During the follicular phase, multiple follicles begin to develop, but only one becomes the dominant follicle. This selection process is influenced by hormone levels, particularly:
- Follicle Stimulating Hormone (FSH): Promotes the growth of follicles.
- Luteinizing Hormone (LH): Plays a role in the final maturation of the dominant follicle.
- Estrogen: As the dominant follicle grows, it produces increasing amounts of estrogen, which helps inhibit the growth of other follicles.
Follicular Atresia
While some follicles mature, others undergo a process called atresia, where they degenerate and are reabsorbed by the body. This is a normal part of the ovarian cycle and ensures that only the healthiest follicles are selected for ovulation. Atresia is essential for maintaining ovarian health and function.
In summary, the follicular development and selection process is crucial for preparing the egg for ovulation and ensuring reproductive success.
Ovulation and Egg Release

LH Surge and Ovulation
Ovulation is a crucial event in the ovarian cycle, typically occurring around the 14th day of a 28-day cycle. This process is primarily triggered by a surge in luteinizing hormone (LH). When estrogen levels rise significantly, they lead to a rapid increase in LH, which causes the most mature follicle to rupture and release an egg. This event marks the transition from the follicular phase to the luteal phase.
Mechanism of Egg Release
The mechanism of egg release involves several steps:
- Follicle Maturation: As follicles grow, they produce estrogen, which prepares the body for ovulation.
- LH Surge: A peak in LH levels triggers the final maturation of the egg and the rupture of the follicle.
- Egg Release: The egg is expelled from the ovary and enters the fallopian tube, where it may encounter sperm for fertilization.
Post-Ovulation Changes
After ovulation, the ruptured follicle transforms into the corpus luteum, which plays a vital role in hormone production. The corpus luteum secretes progesterone and estrogen, which are essential for preparing the uterine lining for a potential pregnancy. If fertilization does not occur, the corpus luteum eventually degenerates, leading to a decrease in hormone levels and the start of a new menstrual cycle.
Luteal Phase and Corpus Luteum Function

Formation of Corpus Luteum
The luteal phase begins right after ovulation and lasts about 12 to 15 days. During this time, the ruptured follicle transforms into a structure known as the corpus luteum. This structure is crucial for preparing the uterus for a potential pregnancy.
Progesterone Production
The corpus luteum produces the hormone progesterone, which plays a vital role in the menstrual cycle. This hormone helps to thicken the lining of the uterus, making it suitable for a fertilized egg. If pregnancy occurs, the corpus luteum continues to produce progesterone for about 10 weeks.
Endometrial Preparation
Under the influence of progesterone, the endometrium (the lining of the uterus) undergoes several changes:
- It becomes more vascularized, providing nutrients to a potential embryo.
- Glands in the endometrium secrete substances that support embryo implantation.
- If no fertilization occurs, the corpus luteum degenerates, leading to a drop in progesterone levels, which triggers the shedding of the endometrial lining.
In summary, the luteal phase is essential for creating a supportive environment for a fertilized egg, and the corpus luteum plays a key role in this process.
Interplay Between Ovarian and Menstrual Cycles
The ovarian and menstrual cycles are closely linked, functioning together to regulate female reproductive health. These cycles typically last between 22 to 32 days, with an average of 28 days.
Synchronization of Cycles
- The ovarian cycle prepares the egg for release, while the menstrual cycle prepares the uterus for potential implantation.
- Hormonal signals from the brain control both cycles, ensuring they work in harmony.
- The phases of the ovarian cycle (follicular, ovulation, and luteal) correspond with specific phases of the menstrual cycle (menstrual, proliferative, and secretory).
Hormonal Interactions
- Follicle Stimulating Hormone (FSH) and Luteinizing Hormone (LH) are crucial for regulating both cycles.
- Estrogen and progesterone levels fluctuate, influencing the uterine lining and the timing of ovulation.
- When a fertilized egg does not implant, hormone levels drop, leading to menstruation and the start of a new cycle.
Impact on Fertility
- Understanding the interplay between these cycles is vital for assessing reproductive health.
- Disruptions in either cycle can affect fertility, making it essential for women to monitor their cycles.
- Lifestyle factors, such as stress and diet, can influence these cycles, highlighting the importance of overall health.
In summary, the ovarian and menstrual cycles are interdependent, with hormonal regulation playing a key role in female reproductive health. This understanding is crucial for women, especially when considering options like period underwear for women to manage menstrual flow.
Clinical Implications of Ovarian Cycle Changes
Understanding the ovarian cycle is crucial for recognizing its impact on reproductive health. The fluctuations in hormone levels throughout the cycle can lead to various clinical implications, including:
Impact on Reproductive Health
- Menstrual irregularities: Changes in the ovarian cycle can result in irregular periods, which may indicate underlying health issues.
- Hormonal imbalances: Disruptions in hormone levels can affect mood, weight, and overall health.
- Fertility challenges: Understanding the cycle is essential for diagnosing and treating fertility issues.
Ovarian Disorders
- Polycystic Ovary Syndrome (PCOS): This condition is characterized by irregular ovulation and can lead to infertility.
- Ovarian cysts: These fluid-filled sacs can form during the cycle and may cause pain or complications.
- Premature ovarian failure: This occurs when the ovaries stop functioning before age 40, affecting hormone levels and fertility.
Fertility Treatments
- Assisted reproductive technologies (ART): Treatments like in vitro fertilization (IVF) rely on understanding the ovarian cycle to optimize egg retrieval and implantation.
- Hormonal therapies: Medications may be used to regulate the cycle and improve fertility outcomes.
- Monitoring cycles: Tracking the ovarian cycle can help in planning for conception and understanding fertility windows.
In summary, the ovarian cycle plays a significant role in female reproductive health, influencing various conditions and treatment options. Menstrual cycle-driven hormone concentrations co-fluctuate with changes in the brain, highlighting the interconnectedness of these systems.
Conclusion
In summary, the ovarian cycle is a crucial part of the female reproductive system, involving a series of changes that prepare the body for potential pregnancy each month. This cycle is divided into three main phases: the follicular phase, ovulation, and the luteal phase. During these phases, hormones like estrogen and progesterone play vital roles in regulating the growth of eggs and the preparation of the uterine lining. Understanding these processes helps us appreciate the complexity of female reproduction and the intricate hormonal interactions that occur. As women age, these cycles eventually lead to menopause, marking the end of reproductive capability. Recognizing these changes can empower women to better understand their bodies and reproductive health.
Frequently Asked Questions
What is the ovarian cycle?
The ovarian cycle is a monthly process that prepares the ovaries to release an egg. It has three main phases: the follicular phase, ovulation, and the luteal phase.
How long does the ovarian cycle last?
The ovarian cycle usually lasts about 28 days, but it can be anywhere from 22 to 32 days.
What happens during ovulation?
During ovulation, a mature egg is released from the ovary. This usually happens around the middle of the cycle.
What hormones are involved in the ovarian cycle?
Key hormones include FSH (Follicle Stimulating Hormone), LH (Luteinizing Hormone), estrogen, and progesterone. These hormones help regulate the cycle.
What is the luteal phase?
The luteal phase is the second half of the ovarian cycle, lasting about 14 days. It prepares the uterus for a possible pregnancy.
How does the ovarian cycle affect menstruation?
The ovarian cycle works alongside the menstrual cycle. If the egg is not fertilized, the cycle ends with menstruation, which is the shedding of the uterine lining.
