Understanding Pelvic Organ Prolapse: Causes and Treatments
Share
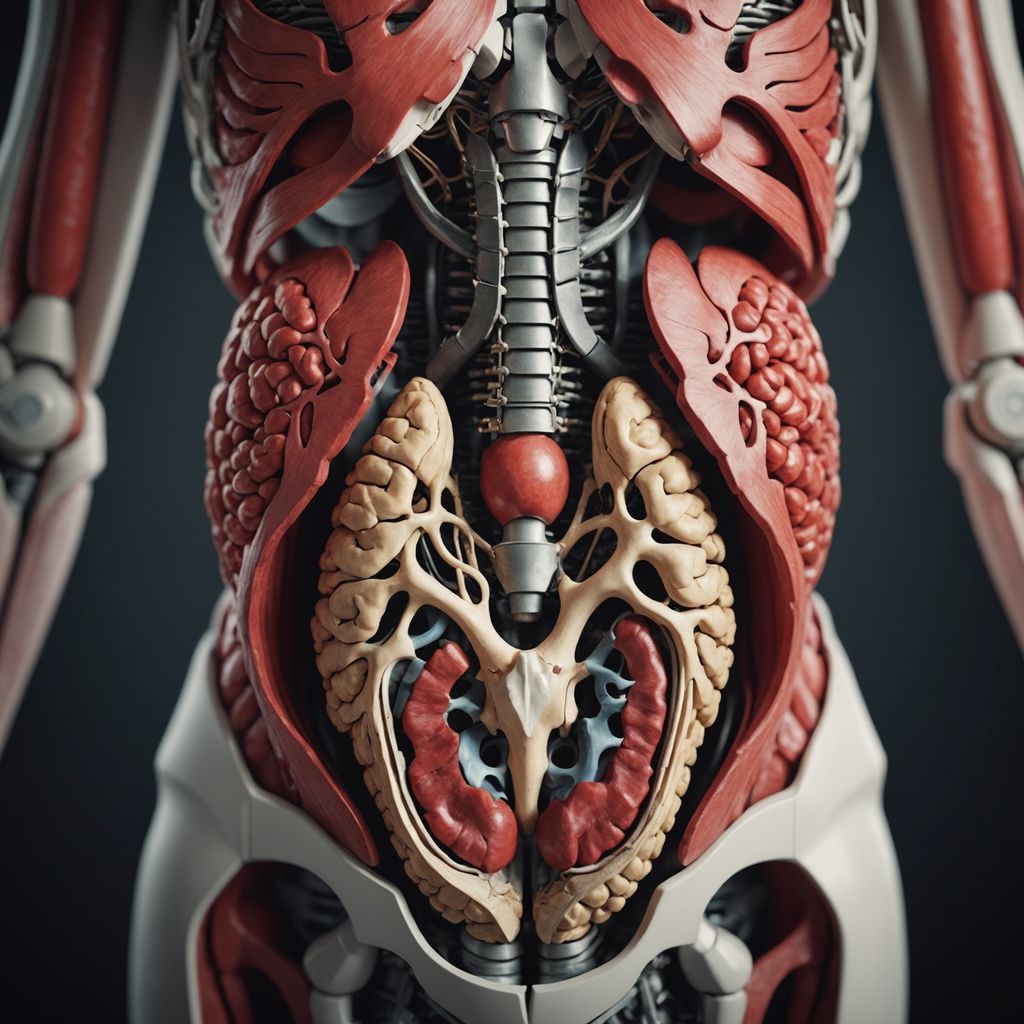
Pelvic organ prolapse (POP) happens when the muscles and tissues in the pelvis weaken, causing organs like the bladder, uterus, or rectum to sag. This condition can affect women of all ages but is more common as they get older. Understanding the causes, symptoms, and treatments can help manage and prevent POP, improving the quality of life for those affected.
Key Takeaways
- Pelvic organ prolapse occurs when pelvic muscles and tissues weaken, causing organs to sag.
- Common causes include pregnancy, childbirth, aging, and obesity.
- Symptoms can range from mild discomfort to severe pain and affect daily activities.
- Nonsurgical treatments like physical therapy and lifestyle changes are often the first steps.
- Surgical options are available for more severe cases or when other treatments fail.
Causes of Pelvic Organ Prolapse

Pregnancy and Childbirth
Pregnancy and childbirth are the most common causes of pelvic organ prolapse. The strain of carrying a baby and the process of giving birth, especially through vaginal delivery, can weaken the pelvic floor muscles. This weakening can lead to the descent of pelvic organs into or outside of the vaginal canal.
Aging and Obesity
Aging naturally weakens the muscles and tissues in the body, including those in the pelvic region. As women age, the risk of pelvic organ prolapse increases. Obesity also contributes to this condition by putting extra pressure on the abdomen, which can strain the pelvic floor muscles over time.
Genetic Factors
Genetics can play a significant role in the likelihood of developing pelvic organ prolapse. Some women may have weaker connective tissues due to their genetic makeup, making them more prone to this condition. If a family history of pelvic organ prolapse or connective tissue disorders exists, the risk may be higher.
Understanding these causes can help in taking preventive measures and seeking appropriate treatments. For more information on managing pelvic health, consider exploring options like period underwear from Trendix, which can offer additional support and comfort.
Symptoms and Diagnosis of Pelvic Organ Prolapse

Common Symptoms
Pelvic organ prolapse can present with a variety of symptoms. The most noticeable symptom is feeling a bulge in the vagina, as if something is falling out. Other symptoms include:
- A sensation of pressure or fullness in the pelvic area
- Lower back pain
- Pain during intercourse
- Urinary issues such as leaking or a constant urge to urinate
- Constipation or loss of bowel control
- Spotting or bleeding from the vagina
In many cases, symptoms are mild in the morning but worsen as the day progresses.
Diagnostic Procedures
To diagnose pelvic organ prolapse, a healthcare provider will review the patient's symptoms and perform a pelvic exam. During the exam, the provider may ask the patient to cough to observe the extent of the prolapse. The examination may be conducted both while lying down and standing up. Often, a pelvic exam is sufficient for diagnosis. Additional tests may include imaging studies or urodynamic tests to assess bladder function.
Severity Assessment
The severity of pelvic organ prolapse is typically assessed using a grading system. This system ranges from mild to severe, based on how far the pelvic organs have descended. The grading helps in determining the appropriate treatment plan. Regular medical check-ups are essential for monitoring the condition and making necessary adjustments to the treatment plan.
Nonsurgical Treatments for Pelvic Organ Prolapse

Nonsurgical treatments for pelvic organ prolapse are often the first line of defense. These treatments aim to manage symptoms and improve quality of life without the need for surgery. Behavioral therapies are a common approach, focusing on exercises like Kegels to strengthen the pelvic floor muscles. These exercises can be guided by a physical therapist who specializes in pelvic health.
Mechanical devices, such as a vaginal pessary, offer another nonsurgical option. A pessary is a removable silicone device that is inserted into the vagina to support the prolapsed organs. This method is particularly useful for those who may not be good candidates for surgery.
Lifestyle modifications can also play a significant role in managing pelvic organ prolapse. Simple changes, such as maintaining a healthy weight and avoiding heavy lifting, can help reduce symptoms. Additionally, wearing specialized period underwear can provide extra support and comfort.
Overall, these nonsurgical treatments provide various options for individuals seeking to manage their condition effectively.
Surgical Treatments for Pelvic Organ Prolapse
Types of Surgical Procedures
When nonsurgical treatments fail to provide relief, surgery may be considered for pelvic organ prolapse. There are two main types of surgical procedures: obliterative and reconstructive. Obliterative surgery involves closing off part or all of the vaginal canal to support the prolapsed organs. Reconstructive surgery, on the other hand, aims to repair and strengthen the pelvic floor tissues, allowing the organs to return to their normal positions.
Risks and Complications
As with any surgery, there are potential risks and complications. These may include infection, bleeding, and damage to surrounding organs. Additionally, there is a chance that the prolapse could recur, especially if the patient undergoes childbirth after the surgery. It's crucial to discuss these risks with a healthcare provider to make an informed decision.
Postoperative Care
Proper postoperative care is essential for a successful recovery. Patients are usually advised to avoid heavy lifting and strenuous activities for several weeks. Follow-up appointments are necessary to monitor healing and address any concerns. Wearing period underwear can provide additional comfort and support during the recovery phase. For more information, visit this link.
Preventive Measures for Pelvic Organ Prolapse
Pelvic organ prolapse can be a challenging condition, but there are several steps that can be taken to reduce the risk. Preventive measures are essential for maintaining pelvic health and avoiding complications.
Lifestyle Changes
Adopting healthy lifestyle habits is crucial. Maintaining a healthy weight can significantly reduce the strain on pelvic organs. Avoiding heavy lifting and managing constipation are also important steps. These changes can help in reducing the risk of prolapse.
Pelvic Floor Exercises
Engaging in regular pelvic floor exercises, such as Kegels, can strengthen the muscles that support the pelvic organs. These exercises are simple and can be done anywhere. They are effective in preventing and managing pelvic organ prolapse.
Regular Medical Check-ups
Regular visits to a healthcare provider can help in early detection and management of pelvic organ prolapse. Routine check-ups allow for timely intervention and can prevent the condition from worsening. It's important to discuss any symptoms or concerns with a healthcare professional.
For women, using period underwear can also provide additional support and comfort. More information on this can be found at period underwear for women.
Impact of Pelvic Organ Prolapse on Quality of Life

Pelvic organ prolapse can significantly affect a person's quality of life. It can lead to physical discomfort, emotional distress, and social challenges. Understanding these impacts is crucial for managing the condition effectively.
Conclusion
Pelvic organ prolapse (POP) is a condition that affects many women, especially as they age or after childbirth. Understanding the causes, such as weakened pelvic muscles, and the various treatment options, from lifestyle changes to surgical interventions, is crucial. Early diagnosis and appropriate management can significantly improve the quality of life for those affected. By working closely with healthcare providers, women can find the best treatment plan tailored to their needs. Awareness and education about POP can lead to better outcomes and help prevent the condition from worsening.
Frequently Asked Questions
What is pelvic organ prolapse?
Pelvic organ prolapse happens when the muscles and tissues supporting the pelvic organs get weak, causing organs like the bladder, uterus, or rectum to drop or press into the vagina.
What causes pelvic organ prolapse?
The main causes are pregnancy and childbirth. Other reasons include aging, being overweight, or having a family history of the condition.
How is pelvic organ prolapse diagnosed?
Doctors use a physical exam and may also do tests like a urine test or use a small tube to look inside the bladder to diagnose pelvic organ prolapse.
What are the symptoms of pelvic organ prolapse?
Common symptoms include a feeling of pressure or fullness in the pelvic area, urinary problems, and discomfort during physical activities.
Can pelvic organ prolapse be treated without surgery?
Yes, nonsurgical treatments include physical therapy, using a pessary (a small plastic device), and making lifestyle changes like losing weight and avoiding heavy lifting.
When is surgery needed for pelvic organ prolapse?
Surgery is usually considered when nonsurgical treatments don't work. The type and severity of the prolapse will help decide the best surgical option.
